First Consensus Meeting on Menopause in the East Asian Region
Osteoporosis: background, pathogenesis, measurement of bone density,
prevention and treatment
Kobchitt Limpaphayom
Department of Obstetrics and Gynaecology, Chulalongkorn University, Bangkok, Thailand
Background
The definition adopted at the Consensus Development Conferences in 1990 and 1993 states that Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture [1, 2]. This definition includes not only established osteoporosis in which fractures have occurred but also preclinical osteoporosis with potential fracture risk.
There are two categories of osteoporosis: primary osteoporosis and secondary osteoporosis. Primary osteoporosis can be divided into three types. Type 1, or postmenopausal osteoporosis, characterized by the disproportionate loss of trabecular bone, is associated with fractures at sites rich in cancellous bone such as the vertebral body and distal radius. Type 2, or age-associated osteoporosis which affects all skeletal sites with both cortical and cancellous bone such as the proximal femur, is a result of senile decline in bone mass. Type 3 is idiopathic osteoporosis which affects premenopausal women as well as middle-aged and young men. Secondary osteoporosis can be caused by an identifiable agent such as glucocorticoids, or by a disease such as hyperthyroidism or myeloma. Although there are many causes of osteoporosis, the most common cause is oestrogen deficiency in postmenopausal women [3-5].
Osteoporotic fracture, which is the major health consequence of this condition, may occur at any skeletal site. However, the primary sites are the spine, hip (proximal femur) and distal forearm [6].
Osteoporosis and its consequence may be regarded as a major source of mortality, morbidity and medical expenditure worldwide [7, 8]. It has been estimated that 75 million people in Europe, Japan and the USA combined are affected by osteoporosis. Furthermore, a significant increase in the age-adjusted incidence of osteoporotic fracture over that past 40-50 years has been reported from many countries. On a worldwide basis, osteoporosis will become an increasing public health problem in the future because the world population is ageing [9, 10]. Riggs and Melton in 1986 [3] reported that approximately 1.3 million fractures cost the US health care system more than 10 billion dollars annually and these occur as the result of osteoporosis.
Pathogenesis
Two factors which affect the probability of developing osteoporosis in later life are the peak bone mass and the rate of bone loss during old age [11]. Bone is formed during the early years of life and the maximum amount of bone in the skeleton will be achieved in the early adult years, by the age of 18-20. Genetics is the major factor determining peak bone mass [12, 13]. However, dietary, hormonal and mechanical factors also contribute to peak bone mass [14]. Disorders of these factors may result in a peak bone mass which is less than optimal. The risks inherent in this situation are of great importance because bone substance achieved during the early years is consumed as the individual advances into old age. At about the age of 50, bone loss occurs at a rate of 0.5-1% annually at most bony sites in both sexes [3]. In postmenopausal women, bone loss occurs at a more rapid rate. The rate may be as much as 3-5% annually in cancellous (trabecular) bone and 1-3% in cortical bone during the early years following the menopause [15]. Although individual patterns of bone loss may vary, the usual pattern is exponential. The rate accelerates in the 5-10 years after the menopause and decreases after that. An approximate total loss of 15% of peak bone mass occurs in the first few postmenopausal years and the lifetime loss may amount to 30-40% [3, 16].
A disturbance of bone remodelling is the underlying mechanism of bone loss [17-20]. Remodelling is a process that couples bone resorption with bone formation, and bone loss occurs when there is increased cellular removal of bone and relatively decreased replacement. In the third or fourth decade of a woman's life, bone mass begins to decline in the hip because of an imbalance between the volume of mineral and matrix removed and that incorporated during the remodelling process.
After the menopause, bone loss occurs predominantly in cancellous bone, which is found in the vertebral bodies and metaphyses of long bones, thus accounting for compression fracture of the vertebra and Colles' fracture in the early menopausal years. The loss of cortical bone occurs at a slower rate because there are fewer sites of remodelling in cortical bone. This senile decline in bone mass occurs in both sexes, although bone loss begins at a later age among men. Fractures that involve the site of primarily cortical bone occur at a later age. Hip fracture is an example of this type of osteoporotic fracture.
There is a strong relationship between bone loss and loss of ovarian production of steroid hormones [21]. As oestradiol production falls in postmenopausal women, loss of bone tissue begins. The underlying mechanism for this relationship is not completely understood. Several studies have suggested that there are oestrogen receptors in cells of osteoblast origin and that oestrogen acts directly on bone cells [22, 23]. However, it appears from recent studies that the effects of oestrogen must be achieved indirectly [24, 25]. Although the dominating pathogenetic factor for osteoporosis in women is oestrogen deficiency, many other factors play a role, such as nutrition, physical activity and chronic illness [26-28]. Certain nutritional and life style factors, such as inadequate intake of calcium, may contribute to low bone mass independent of oestrogen level, and this can further increase a woman's risk of developing postmenopausal osteoporosis [29-31].
Although the relationship between bone mass and osteoporotic fracture is established, it is not inevitable that every osteoporotic patient will sustain fractures. The occurrence of fractures depends not only on bone fragility but also on the degree of trauma experienced [6, 32]. Usually, osteoporotic fractures are associated with a fall to the floor, to which elderly people have an increased tendency [33-35]. There are a number of causes of increased tendency to falls in old age, such as reduced visual acuity, vestibular dysfunction, dementia, musculoskeletal disorders and use of medication [36]. However, severe postural hypotension is often a dominant feature [37].
Measurement of bone mass density
Bone mass density (BMD) measurement is indicated whenever a clinical decision to intervene with an agent will be directly influenced by the outcome of the tests. When osteoporosis is suspected, BMD measurement is the single best diagnostic tool because it helps the physician determine fracture risk and identify patients who are candidates for intervention, Kanis et al. [38] reported that for every decrease in bone mass of 1 standard deviation (SD), the relative risk of fracture increases 1.5- to 3-fold.
Bone fragility is closely correlated with reduced bone mineral which can be measured by a number of different techniques [39]. Until recently, the only way to estimate the amount of bone mass was to take regular x-rays of the skeleton [40]. Conventional x-ray is very insensitive and bone loss is not recognized until around 25-30% of bone density has been lost [41], by which time osteoporosis has developed and the patient often has suffered a number of fractures and therapeutic intervention may be too late. The main role of conventional x-ray today is for the diagnosis of fractures secondary to osteoporosis.
During the last two decades more advanced technology for determining bone mass has been developed and several techniques are available. With these techniques of bone densitometry, the clinician can detect low bone mass prior to fracture. This will benefit in the early treatment of osteoporosis and the prevention of osteoporotic fracture.
BMD measurements should be performed in the following settings:
— for risk assessment in peri- or postmenopausal women who are concerned about osteoporosis and who are willing to accept available interventions;
— in women with x-ray findings that suggest the presence of osteoporosis;
— in women beginning or receiving long-term glucocorticoid therapy, provided intervention is an option;
— for perimenopausal or postmenopausal women with asymptomatic primary hyperparathyroidism in whom evidence of skeletal loss would result in parathyroidectomy;
— in women undergoing treatment for osteoporosis, as a tool for monitoring the therapeutic response.
Some women who have had several low-trauma fractures and a radiographic diagnosis of osteoporosis can be diagnosed without BMD measurement; however, the only effective way to monitor therapy objectively is by comparison with a baseline BMD measurement. BMD measurement is not indicated in women who are receiving oestrogen therapy for non-skeletal indications and who do not have fragility fractures.
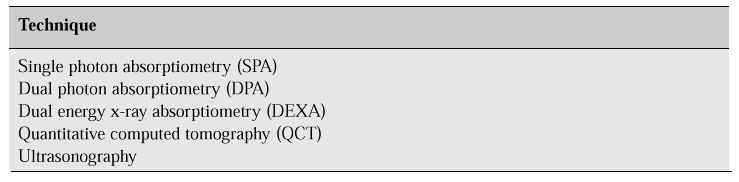
Table I shows the techniques available for estimating bone mass. All rely on the alteration of an external signal by hard tissue, which absorbs more of the energy than soft tissue.
Table I: Techniques for estimating bone mass.
Single photon absorptiometry [41-43]
The technique of single photon absorptiometry (SPA) involves the passing of a collimated beam of low-energy photons from a 125I-source through a limb and measuring the transmitted radiation using a sodium iodide scintillation detector. Differential photon absorption between bone and a uniform layer of soft tissue around it allows calculation of bone mineral in the path of the beam, expressed in grams per centime-tre squared when normalized for bone diameter. In clinical practice, areas of the appendicular skeleton, such as the radius or calcaneous, are measured. This method cannot differentiate between cortical and trabecular bone, and interference from surrounding tissue limits its use to measurement of peripheral sites such as the distal or mid-radius.
SPA is accurate and very precise. Precision error (the extent to which repeated measurements differ; also called reliability or reproducibility) is low at the mid-radius, making this technique particularly useful for serial measurements in the same individual. However, short-term changes in bone mineral content at this diaphyseal site are typically of small magnitude. Change is more rapid in the cancellous bone of the metaphysis, but precision there is somewhat lower because of inexact repositioning of the limb on subsequent scans. Accuracy error (the extent to which the measurement differs from the true state; also called validity) is about 5% and results from technical factors within the system and from variations in soft tissue, especially fat within and around the bone. Bone mineral content in the radius or os calcis is correlated with bone mineral in the spine and hip but does not accurately reflect bone mass at the other sites in individual patients. Nonetheless, as noted above, SPA measurements allow stratification of patients on the basis of their overall fracture risk.
SPA has been used for more than 20 years. The technique takes only about 15 min and the cost is low. However, its main drawback is the inability to assess bone mineral of the hip or spine.
Dual photon absorptiometry [41-43]
Dual photon absorptiometry (DPA) is a direct extension of SPA, but uses 153Gd as a source, and measures bone density by determining the absorption of two beams of photons at two different energies. It is therefore able to measure bone density (as mass per area) in the proximal femur and lumbar spine, as well as the total body. However, it cannot differentiate between cortical and trabecular bone at each site. In the lumbar spine, the scan area generally covers L2-L4 and includes bone in the vertebral bodies and posterior elements but not the transverse processes. Results are usually expressed as grams per unit area scanned. For the proximal femur, bone mineral density is estimated at three anatomical regions: the femoral neck, Ward's triangle (an area within the proximal femur containing a large amount of trabecular bone) and the trochanteric region. Precision for this technique for both spine and hip measurements is of the order of 2-4%.
The scanning time is significantly longer than for SPA; for hip and spine measurements it takes about 20 min for each site.
Dual energy x-ray absorptiometry [41-43]
Dual energy x-ray absorptiometry (DEXA) is similar to DPA, but the radioisotope source is replaced by an x-ray source. This obviates the problem of decay of isotope sources, but more important, the greater photon flux permits scan times to be speeded up considerably without loss of precision. Beam collimation is also tighter, with higher spatial resolution as a result. DEXA equipment can make the same measurements that are possible with DPA, i.e. spine, hip, specific skeletal regions or total body, with a precision error of about 1-2%. Accuracy error is comparable to DPA, ranging from 4 to 10% depending on skeletal site, and some improvement relative to conventional DPA may result from the capability to scan the lumbar spine laterally.
The scanning time for DEXA is shorter than for DPA (approximately 5 min at each site) and the radiation dose is less. Furthermore, DEXA machines also appear to be easier to use, with less operator interaction. The radiation exposure at a distance of one metre from the equipment is less then 1 mR. No additional shielding is necessary for the patient operator in the room.
Quantitative computed tomography [41-43]
Quantitative computed tomography (QCT) is an extension of the computed tomography imaging approach that quantifies the absorption of ionizing radiation by calcified tissue. Measurements, usually from a single energy x-ray source, are compared with a standard reference material (such as K2HPO4) to calculate bone mineral equivalents. This technique measures true density and results are expressed as milligrams of K2HPO4 per cubic centimetre of bone volume, thus reflecting three-dimensional density rather than the two-dimensional areal density of DPA and DEXA.
Advantages of QCT are that trabecular bone can be distinguished from cortical bone, and extraosseous calcium, which will artificially elevate the bone density measured by DEXA, can be readily identified. The disadvantages with this technique are the high radiation dose and poorer accuracy and reproducibility (6-8%) compared with DPA and DEXA. Patient acceptability of QCT is good, but the expense is higher than with the other techniques. Consequently, QCT is less desirable for serial measurements. Scans take about 15 min and can be programmed on a variety of QCT devices. However, machines dedicated to bone mineral measurement generally produce the best results.
Correlations of bone mineral density among various measurements carried out at Chulalongkorn Hospital revealed a significant correlation of distal and ultradistal part of the forearm with spine (r = 0.619, p < 0.001) and with hip (r = 0.602, p < 0.001), which can be applied in mass screening programmes in any country [44].
Ultrasonography [41-43]
While bone density is a useful clinical predictor of fracture risk, other factors are also important. Such factors may include the intangible ‘quality' of bone including the trabecular architecture of bone. Perforations in trabecular bone may lead to a decrease in the continuity or ‘connectivity' of bone and lead to a compromise in its architectural integrity. Although this architecture cannot be analysed by densitometric techniques, there is some evidence that transmission of sound waves through bone may reflect not only the bone mineral content but also the architectural properties and ‘connectivity' of the trabecular bone. Broadband ultrasonic attenuation (BUA) describes the increase in ultrasound attenuation over a particular frequency range, typically 0.2-0.6 MHz, and may be used to estimate bone density of the calcaneus [45]. The heel is placed in a small water bath between two ultrasonic transducers at a fixed separation. One transducer acts as a transmitter, the other as a receiver. The measurement takes between 1 and 10 min, depending on the machinery used, and involves no ionizing radiation.
Several studies have shown significant correlations between calcaneus BUA and spine or hip density measured by DEXA and DPA. Further prospective data are clearly required in this area. Bone ultrasound scanners are now becoming commercially available and may become useful screening tools since they avoid the use of ionizing radiation and may be less expensive.
Poshyachinda and Chaiwatanarat [46] reported that in Thai women, BMD increases from the age of 20 and peaks at around the age of 35 at both the anterior and lateral lumbar spines and the femoral neck, and bone loss begins at the age of 40. Accelerated bone loss was observed between the age of 50 and 65 years.
Magnitude of the problem
The prevalence of osteoporosis of both the lumbar spine and femoral neck is 15.7 and 9.5%, respectively, according to hospital-based data [47]. There are no risk factors detected in the premenopause with regard to the spine or femoral neck. In the postmenopause, age above 60 years and low body mass index are significant risk factors in both the spine and femoral neck. Years since the menopause are associated with osteoporosis only in the spine.
Prevention of osteoporosis
Prevention is the most effective approach to osteoporosis. This may be done by optimizing peak bone mass at skeletal maturity, by preventing bone loss, or by restoring the bone mineral and architecture in osteoporotic bone.
Diagnostic criteria
The World Health Organization has established the following BMD-based diagnostic criteria for women who have experienced no fragility fractures [48]. These criteria provide the physician with a basic diagnostic framework and should not serve as a precept for the therapeutic decision.
— normal: a BMD value within 1 SD of the young adult mean;
— osteopenia: a BMD value more 1 SD but less than 2.5 SD below the young adult mean;
— osteoporosis: a BMD value 2.5 SD or more below the young adult mean.
The patient with one or more low-trauma fractures is considered to have osteopo-rosis, regardless of the BMD value.
Most bone densitometry reports designate the SDs from the normal young adult mean in the form of ‘T' scores. Diagnostic criteria are commonly stated as T scores because fracture risk is derived from epidemiologic studies that use this designation as a reference. The densitometry reports also provide ‘Z' scores, which represent the SDs from age- and sex-matched control subjects. The Z score can provide useful diagnostic information because a Z score of 2 or more below the age- and sex-matched control may suggest a secondary cause of osteoporosis. For each 10% decrease in BMD, the fracture risk approximately doubles.
Measurement sites
BMD measurement at any axial (i.e. hip, vertebra) or peripheral (i.e. radius, calcaneus) site is useful for a one-time assessment of fracture risk. Currently, however, the American Association of Clinical Endocrinologists recommends performing the first measurement when therapeutic intervention is planned. Vertebral compression and the presence of spinal implants, degenerative arthritis, or other spinal conditions can falsify the BMD measurement. Ideally, if resources allow, measurements should be taken at both sites for baseline and follow-up because the trabecular bone of the spine produces the quickest therapeutic response [49].
Optimizing peak bone mass
Peak bone mass is primarily under genetic control; however, during growth the amount of bone tissue that is deposited within the skeleton may be modified by diet, life style or the presence of chronic disease [13].
There is no doubt that bone mass at skeletal maturity can be improved by optimizing the diet, i.e. by ensuring a reasonable intake especially of calcium but also of protein, carbohydrates, fat and other nutrients. Exercise, as well as abstinence from tobacco, alcohol and drugs, is also beneficial for the skeleton as it is for the whole body.
Puberty is also an important factor in skeletal development. It is during this stage of life that the differences in skeletal size and diversity between the sexes become maximal. Achievement and maintenance of regular cyclic ovarian function are crucial to skeletal health in women. Any ovarian dysfunction results in bone loss and must be investigated and treated to avert the possibility of osteoporotic fracture.
Patient acceptance of proposed treatment
The physician should inform the patient of all the risks and benefits associated with intervention, and the patient should make a decision based on this information.
Prevention of bone loss
Calcium
Calcium is significant for creating optimum bone mass [50]. It is important for both skeletal development during childhood and adolescence and maintenance of a high bone quality in adults [30].
It has been shown in several clinical trials that calcium supplementation can reduce postmenopausal bone loss and fractures [51-54]. However, the benefits are greatest in women who are more than 5 years beyond the menopause. It is not sufficient to slow bone loss in the first 5 years of the postmenopausal period by calcium supplementation alone because bone loss during the early postmenopausal years is primarily due to oestrogen deficiency.
It is recommended that postmenopausal women should increase their calcium intake to 1000-1500 mg per day [55, 56]. Calcium is a nutrient and should be obtained from dietary sources; however, a supplement may be used if dietary calcium is inadequate.
Calcium supplements should be taken together with a meal either once at the end of the day or twice a day and each dose should not exceed 500-700 mg. The supplement should be taken together with plenty of water (one to two glasses). The daily calcium intake (i.e. dietary plus supplements) should not exceed 1000-1500 mg. At this level it is unlikely to produce any side effects. However, if the patient has a history of kidney stones, a high calcium intake is not advised without proper investigation [57].
Vitamin D
The metabolites of vitamin D are important in the regulation of calcium metabolism. Vitamin D deficiency with decreased serum levels of the active metabolite, 1,25-vitamin D, results in rickets in children and osteomalacia in adults. For many people, the most important source of vitamin D is sunlight. Thirty minutes of direct exposure to sunlight daily will ensure adequate vitamin D production in the skin. People living in northern latitudes or who for traditional or other reasons are only rarely exposed to the sun are more dependent on dietary sources of vitamin D. Vitamin D is found in abundant amounts only in fish liver oils and in smaller amounts in oily salt-water fish, egg, butter, margarine and milk. For many people, a daily vitamin D supplement will therefore be necessary to reach the intake which will prevent vitamin D deficiency. The daily intake should not exceed the recommended allowance. In the USA, it is recommended to supplement the diet of elderly people with 800 IU of vitamin D [58]. Several clinical trials from developed countries have shown that vitamin D supplementation in elderly people can reduce bone loss and fractures [52, 56, 59].
Oestrogen
Many studies have demonstrated that oestrogen intervention reduces the rate of bone loss among postmenopausal women [60]. The study of longest duration demonstrated that oestrogen intervention stopped peripheral bone loss for at least 10 years. The effect persisted for as long as therapy was given and when treatment was stopped bone loss began again [61]. The bone loss that had been prevented was not rapidly lost when the treatment was stopped. It recurred after stopping oestrogen therapy at the same rate as it was just before therapy was instituted. Retardation of bone loss was seen even when intervention was delayed for several years after menopause. However, maximum benefit is achieved when intervention is begun as soon as possible after ovarian function ceases. The minimum effective dose for oral conjugated equine oestrogen appears to be 0.625 mg/day [62]. Other oestrogens are also effective in prevention, whether delivered by oral or non-oral routes [63, 64].
A number of epidemiological studies have further shown that oestrogen therapy decreases the number of osteoporotic fractures in postmenopausal women [65-68]. The majority of studies have examined the effects of oestrogen on the risk of hip fracture, and the general conclusion appears to be that oestrogen intervention reduces the risk of hip fracture by about 50%. Similar data exist for fractures of the distal radius. The data are more sparse for vertebral fracture. One epidemiological study has shown that oestrogens provide considerable protection [60], and one controlled trial demonstrated that long-term oestrogen reduces the appearance of vertebral radiological deformities [69], assumed to be the precursor of vertebral fractures. Thus, the bulk of evidence suggests that long-term oestrogen intervention will reduce the risk of all osteoporotic fractures significantly among the ageing female population.
Treatment
Goals for therapy should be specific such as: preventing fractures, stabilizing or increasing bone mass, relieving symptoms of fractures and skeletal deformities, and lastly maximizing physical function.
Restoration of the osteoporotic skeleton is difficult. There are few medical possibilities for severe osteoporosis with fractures. However, if the diagnosis is made when bone mass has only decreased to a limited extent, there are more therapeutic options. Drug treatment for osteoporosis may retard bone loss or stimulate bone formation. In all patients, environmental factors that may aggravate the bone loss or increase the risk of fracture should be eliminated.
Vitamin D
Longitudinal studies of women passing from the premenopausal to the postmenopausal state have failed to demonstrate any changes in serum concentrations of the vitamin D metabolites [70]. However, a study in the USA has shown that serum levels of vitamin D decline with age, and living in northern latitudes, values in young adults are generally above 100 nmol/l, but for people above 80 years of age, the values are often below 30 nmol/l [56]. There is evidence from many clinical trials that vitamin D or its analogues have little or no effect on postmenopausal bone loss or bone mass in osteoporotic patients. Nevertheless, several studies from Denmark and Japan have demonstrated an effect of 1a-vitamin D on bone mass and on fracture frequency [70, 71]. The response may depend on the patients selected and those patients with the most severe degree of osteoporosis had the best response. In a large study in New Zealand, calcitriol was shown to significantly reduce fracture in comparison with calcium supplement [72].
Oestrogens
Oestrogens can stop bone loss whether the women is 50, 60 or 70 years old [70]. For many years it was considered useless to start a late-postmenopausal woman on oestrogen therapy because studies showed that oestrogens only stopped further bone loss but did not increase bone mass. Moreover, it was inconvenient for women who had had no periods for more than 10 years to experience regular bleeding again.
However, recent clinical studies have found an increase in bone density in the lumbar spine and femur of postmenopausal women taking oestrogens [47, 72]. All routes of oestrogen administration have been shown to be effective [63, 64]. Furthermore, the new continuous combined oestrogen/progestogen treatment does not induce vaginal bleeding. This is especially true of those elderly women who have had an atrophic endometrium for many years. This makes hormone therapy a practical treatment for patients with symptomatic osteoporosis.
The addition of progestogens does not reduce the efficacy of oestrogens; nandrolone derivatives may actually enhance the skeletal response [73].
Calcitonin
Calcitonin directly suppresses the activity of osteoclasts and also inhibits their recruitment [74]. It has been isolated from a large number of animal species. The fish calcitonins are the most resistant to degradation in man, and thus have the greatest potency per unit weight. It is not known whether other species of calcitonins will prove to be more effective.
The literature contains numerous studies on the effects of calcitonin treatment in patients with osteoporosis. The overall result is that treatment with calcitonin (by injection and nasal spray) stops further bone loss in patients with symptomatic osteoporosis. There is no conclusive evidence, however, that calcitonin therapy results in any substantial increase in bone mass except in the subset of patients with high bone turnover, and there are no data on the long-term effect on either bone mass or fracture rate. Calcitonin has, however, been approved in many countries for the treatment of patients with symptomatic osteoporosis [70, 75].
In established osteoporosis, bone pain is one of the major complaints. Calcitonin has significant analgesic effects, reducing the duration of confinement to bed and decreasing the need for concomitant analgesics [76].
Bisphosphonates
Bisphosphonates are stable analogues of pyrophosphate which bind to the bone surface and inhibit osteoclastic activity. Etidronate disodium has been shown to increase bone density in women with spinal osteoporosis compared with a group of placebo-treated controls, who lost bone density. The incidence of new fractures in the treated women in one study was less than that in controls [77, 78].
Newer and more potent bisphosphonates such as tiludronate and aminohydroxypropylidene diphosphonate have been developed. Aminohydroxypropylidene diphosphonate given continuously has been shown to cause a mean rise in lumbar bone density of approximately 3% per year; in some patients the density increased by 50% after 4 years of treatment [79, 80].
Bisphosphonates have emerged as a novel class of non-hormonal compounds available to treat osteoporosis. Further research may prove bisphosphonates beneficial for the prevention as well as active treatment of this condition.
Fluoride
Fluoride stimulates bone formation by increasing the population of the osteoblast and thereby significantly increasing bone mass [81]. Many studies have confirmed that sodium fluoride or monofluorophosphates can increase bone density, particularly at the lumbar spine. Vertebral fracture rates can be reduced if appropriate doses are selected [16, 82, 83]. The effect on cortical bone is much less marked. The new bone mass that is formed is different from normal bone but it seems to have a certain strength. When fluoride is given alone in large therapeutic doses, there is a pronounced impairment of mineralization, leading to histologic osteomalacia. Concurrent administration of calcium and vitamin D, however, largely offsets this effect [70].
The response to fluoride varies considerably between patients. Those with younger bone show the least response, perhaps because bone cell activity in these subjects is already high and therefore less able to be increased [84]. In several large series of patients treated with fluoride, 30-50% experienced significant adverse effects. The most frequent were gastric irritation and a lower extremity pain syndrome. The gastric symptoms comprised pain, nausea, vomiting, and occasionally, blood loss causing anaemia [70].
The effects of fluoride on cortical bone are still being debated. The incidence of hip fracture was shown in some studies to increase in fluoride-treated patients [86, 87]. However, several controlled trials did not find any change in the rate of hip fracture in fluoride-treated groups [82, 83].
In view of its variable response to treatment and the side effects, the treatment of osteoporosis with fluoride is recommended only in specialist centres.
Conclusion and recommendations
The physician should perform annual follow-up assessments of all high-risk patients and patients who are part of any osteoporosis prevention or treatment programme. Follow-up assessment should include the following:
— a complete history;
— a complete medical examination, including breast and pelvic examinations;
— mammography and Pap smear if indicated;
— assessment of compliance and activity level;
— assessment of stature;
— reinforcement of the therapeutic programme and evaluation of the patient's level of understanding and concern.
The physician should use follow-up BMD measurements to monitor changes in bone mass. Using the DEXA technique, a change of 5% is considered clinically significant and is usually not observed in less than 2 years.
The following follow-up bone measurements are recommended:
— normal BMD (T score <1.5): every 2-3 years;
— osteoporosis prevention: every 1-2 years until bone mass stabilizes, then every 2-3 years;
— therapeutic programme: every year for 3 consecutive years, then measurement every 2 years.
For the medical evaluation, an annual check-up is essential for all patients. The evaluation must include a pelvic examination, breast examination and, if indicated, a mammography and Pap smear. For all patients who continue oestrogen therapy, endometrial biopsy, transvaginal ultrasonography or dilatation and curettage are indicated to rule out neoplastic disorders whenever prolonged (>10 days) or persistent, irregular uterine bleeding occurs.
References
1. Consensus Development Conference. Prophylaxis and treatment of osteoporosis. Am J Med 1991; 90: 107-10.
2. Consensus Development Conference. Diagnosis, prophylaxis and treatment of osteoporosis. Am J Med 1993; 94: 646-50.
3. Riggs BL, Melton LJ III. Involutional osteoporosis. N Engl J Med 1986; 314: 1676-84.
4. Melton LJ III, Riggs BL. Clinical spectrum. In: Riggs BL, Melton LJ III, eds. Osteoporosis: etiology, diagnosis and management. New York: Raven Press; 1988:155-79.
5. Aitken M. Osteoporosis in clinical practice. Bristol, UK: John Wright; 1984.
6. Melton LJ III. Epidemiology of fractures. In: Riggs BL, Melton LJ III, eds. Osteoporosis: etiology, diagnosis and management. New York: Raven Press; 1988: 133-54.
7. Garraway WM, Stauffer RN, Kurland LT, O'Fallon WM. Limb fractures in a defined population. II. Orthopedic treatment and utilization of health care. Mayo Clin Proc 1979; 54: 708-13.
8. Holbrook TL, Grazier K, Kelsey JL, Stauffer RN. The frequency of occurrence, impact and cost of selected musculoskeletal conditions in the United States. Chicago, IL: American Academy of Orthopedic Surgeons; 1984.
9. Cooper C, Fogelman I, Melton LJ III. Bisphosphonates and vertebral fracture: an epidemiological perspective. Osteoporosis Int 1991; 2: 1-4.
10. Cummings SR, Kelsey JL, Nevitt MC et al. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev 1985; 7: 178.
11. Hui SL, Slemenda CW, Johnston CC Jr. The contribution of bone loss to postmenopausal osteoporosis. N Engl J Med 1990; 1: 30-4.
12. Kelly PJ, Eisman JA, Sambrook PN. Interaction of genetic and environmental influences on peak bone density. Osteoporosis Int 1990; 1: 56-60.
13. Smith DM, Nance WE, Kang KW et al. Genetic factors in determining bone mass. J Clin Invest 1973; 52: 2800-8.
14. Burckhardt P, Michel CH. The peak bone mass concept. Clin Rheumatol 1989; 8 (suppl 2): 16-21.
15. Stevenson JC, Banks LM, Spinks TJ et al. Regional and total skeletal measurements in the early postmenopause. J Clin Invest 1987; 80: 258-62.
16. Wark JD. Osteoporosis: pathogenesis, diagnosis, prevention and management. Bailliere's Clin Endocrinol Metab 1993; 7: 151-81.
17. Dempster DW, Shane E, Horbert W, Lindsay R. A simple method for correlative light and scanning electron microscopy of human iliac crest bone biopsies: qualitative observations in normal and osteoporotic subjects. J Bone Miner Res 1986; 1: 15-21.
18. Heaney RP, Recker RR, Saville PD. Menopausal changes in bone remodeling. J Lab Clin Med 1978; 92: 964-70.
19. Melton LJ III, Chao EYS, Lane J. Biomechanical aspects of fractures. In: Riggs BL, Melton LJ III, eds. Osteoporosis: etiology, diagnosis, and management. New York: Raven Press; 1988: 111-31.
20. Parfitt AM. Bone remodeling: relationship to the amount and structure of bone, and the pathogenesis and prevention of fractures. In: Riggs BL, Melton LJ III, eds. Osteoporosis: etiology, diagnosis and management. New York: Raven Press; 1988: 45-93.
21. Lindsay R. Sex steroids in the pathogenesis and prevention of osteoporosis. In: Riggs BL, Melton LJ III, eds. Osteoporosis: etiology, diagnosis and management. New York: Raven Press, 1988; 333-58.
22. Eriksen EF, Colvard DS, Berg NJ et al. Evidence of estrogen receptors in normal human osteoblast-like cells. Science 1988; 241/4861: 84-6.
23. Komm BS, Terpening CM, Benz DJ et al. Estrogen binding, receptor mRNA, and biologic response in osteoblast-like osteosarcoma cells. Science 1988; 241/4861: 81-4.
24. Cosman F, Shen V, Xie F et al. Estrogen protection against bone resorbing effects of parathyroid hormone infusion. Assessment by use of biochemical markers. Ann Intern Med 1993; 118/5: 337-43.
25. McSheehy PM, Chambers TJ. Osteoblastic cells mediate osteoclastic responsiveness to parathyroid hormone. Endocrinology 1986; 118/2: 824-8.
26. Krolner B, Toft B. Vertebral bone loss: an unheeded side effect of therapeutic bed rest. Clin Sci 1983; 64: 537-40.
27. Nordin BEC. The pathogenesis of osteoporosis. Lancet 1961; ii: 1011-5.
28. Pocock N, Eisman J, Gwinn T et al. Muscle strength, physical fitness, and weight but not age predict femoral neck bone mass. J Bone Miner Res 1989; 4: 441-8.
29. Heaney RP. Nutritional factors in bone health in elderly subjects: methodological and contextual problems. Am J Clin Nutr 1989; 50 (suppl 5): 1182-9.
30. Heaney RP. Nutritional factors in bone health. In: Riggs BL, Melton LJ III, eds. Osteoporosis: etiology, diagnosis and management. New York: Raven Press; 1988: 359-72.
31. Riggs BL, Melton LJ III. Involutional osteoporosis. In: Evans JG, Williams TF, eds. Oxford textbook of geriatric medicine. Oxford: Oxford University Press; 1992: 405-11.
32. Riggs BL. Practical management of the patient with osteoporosis. In: Riggs BL, Melton LJ III, eds. Osteoporosis: etiology, diagnosis and management. New York: Raven Press; 1988: 481-90.
33. Cummings SR, Nevitt MC. Epidemiology of hip fractures and falls. In: Kleerekoper M, Krane SM, eds. Clinical disorders of bone and mineral metabolism. New York: Liebert, 1989; 231-3.
34. Gryfe CI, Amies A, Ashley MJ. A longitudinal study of falls in an elderly population. I. Incidence and morbidity. Age Ageing 1977; 6: 201-10.
35. Gibson MJ. The prevention of falls in late life. Dan Med Bull 1987; 34 (suppl 4): 1-24.
36. Nguyen T, Sambrook P, Kelly P et al. Prediction of osteoporotic fractures by postural instability and bone density. Br Med J 1993; 307: 111-5.
37. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988; 319: 1701-7.
38. Kanis J, Melton LJ III, Christiansen C et al. The diagnosis of osteoporosis. J Bone Miner Res 1994; 3: 1137-41.
39. Hui SL, Slemenda CW, Johnston CC Jr. Baseline measurement of bone mass predicts fracture in white women. Ann Intern Med 1989; 111: 355-61.
40. Genant HK, Bogler JB, Block JE. Radiology of osteoporosis. In: Riggs BL, Melton LJ III, eds. Osteoporosis: etiology, diagnosis and management. New York: Raven Press; 1988: 181-220.
41. Stevenson JC, Marsh MS. An atlas of osteoporosis. Park Ridge, IL: Parthenon, 1992; 27-9.
42. Melton LJ III, Wahner HW, Delmas PD. Bone mineral measurement and biochemical markers of bone cell function. In: Lorrain J, ed. Comprehensive management of menopause. New York: Springer; 1994: 97-109.
43. Lindsay R, Kelly P. Osteoporosis in postmenopausal women. In: Wren BG, Nachtigall LE, eds. Clinical management of the menopause. Sydney: McGraw-Hill, 1996; 86-105.
44. Limpaphayom K, Bunyavejchevin B, Taechakraichana N. Similarity of bone mass measurement among hip, spines and distal forearm. J Med Assoc Thai 1998; 81: 94-7.
45. Agren M, Karellas A, Leahey D et al. Ultrasound attenuation of the calcaneus: a sensitive and specific discriminator of osteopenia in postmenopausal women. Calcif Tissue Int 1991; 48: 240-4.
46. Poshyachinda M, Chaiwatanarat T. Assessment of bone mineral density in normal Thais. Asian J Radiol 1996; 11/1: 1-12.
47. Limpaphayom K, Taechakraichana N, Poshyachinda M, Jaisamrarn U. Bone changes in postmenopausal Thai women with or without hormonal replacement therapy. J Med Assoc Thai 1995; 78/11: 573-7.
48. Bell NH, Skary J, Stevens J et al. Demonstration that bone mass is greater in black than in white children. J Bone Miner Res 1991; 6: 719-23.
49. Wahner HW, Donn WL, Riggs BL. Assessment of bone mineral (part 2). J Nucl Med 1984; 25: 1241-53.
50. Sowers MF, Wallace RB, Lemke JH. Correlates of forearm bone mass among women during maximal bone mineralization. Prev Med 1985; 14: 585-96.
51. Dawson-Hughes B, Dallal GE, Krall EA, et al. A controlled trial of the effect of calcium supplementation on bone density in postmenopausal women. N Engl J Med 1990; 323: 878-83.
52. Chapuy MC Arlot ME, Duboeuf F, et al. Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med 1992; 327: 1637-42.
53. Reid IR Ames RW, Evans MC, et al. Effect of calcium supplementation on bone loss in postmenopausal women. N Engl J Med 1993; 328: 460-4.
54. Elders PJ, Netelenbos JC, Lips P, et al. Calcium supplementation reduces vertebral bone loss in perimenopausal women: a controlled trial in 248 women between 46 and 55 years of age. J Clin Endocrinol Metab 1991; 73: 533-40.
55. Heaney RP, Recker RR, Saville PD. Calcium balance and calcium requirements in middle-aged women. Am J Clin Nutr 1977; 30/10: 1603-11.
56. Heaney RP. Bone mass, nutrition, and other lifestyle factors. Am J Med 1993; 95 (suppl 5a): 29-33.
57. Christiansen C, Riis BJ. Postmenopausal osteoporosis. Alborg, Denmark: Handelstrykkeriet; 1990: 53-65.
58. Parfitt AM, Gallagher JC, Heaney RP, et al. Vitamin D and bone health in the elderly. Am J Clin Nutr 1982; 36 (suppl 5): 1014-31.
59. Heikinheimo RJ, Inkovaara A, Harju EJ, et al. Annual injection of vitamin D and fractures of aged bones. Calcif Tissue Int 1992; 51: 105-10.
60. Ettinger B, Genant HK, Cann CE. Long-term estrogen replacement therapy prevents bone loss and fractures. Ann Intern Med 1985; 102/3: 319-24.
61. Lindsay R, Hart DM, MacLean A et al. Bone response to termination of oestrogen treatment. Lancet 1978; i/8078: 1325-7.
62. Lindsay R, Hart DM, Clark DM. The minimum effective dose of estrogen for prevention of postmenopausal bone loss. Obstet Gynecol 1984; 63/6: 759-63.
63. Riis BJ, Thomsen K, Strom V, Christiansen C. The effect of percutaneous estradiol and natural progesterone on postmenopausal bone loss. Am J Obstet Gynecol 1987; 156: 61-5.
64. Stevenson JC, Cust MP, Gangar KF et al. Effects of transdermal versus oral hormone replacement therapy on bone density in spine and proximal femur in postmenopausal women. Lancet 1990; 336/8710: 265-9.
65. Hutchinson TA, Polansky SM, Feinstein AR. Post-menopausal oestrogens protect against fractures of hip and distal radius. A case-control study. Lancet 1979; ii/8145: 705-9.
66. Kreiger N, Kelsey JL, Holford TR, O'Connor T. An epidemiologic study of hip fracture in postmenopausal women. Am J Epidemiol 1982; 116/1: 141-8.
67. Naessen T, Persson I, Adami HO et al. Hormone replacement therapy and the risk for first hip fracture. A prospective, population-based cohort study. Ann Intern Med 1990; 113: 95-103.
68. Weiss NS, Ure CL, Ballard JH et al. Decreased risk of fractures of the hip and lower forearm with postmenopausal use of estrogen. N Engl J Med 1980; 303: 1195-8.
69. Lindsay R, Hart DM, Forrest C, Baird C. Prevention of spinal osteoporosis in oophorectomised women. Lancet 1980; ii/8205: 1151-4.
70. Christiansen C, Riis BJ. Postmenopausal osteoporosis. Alborg, Denmark: Handelstrykkeriet, 1990; 66-75.
71. Shiraki M, Orimo H, Ito H et al. Long-term treatment of postmenopausal osteoporosis with active vitamin D3, 1-alpha-hydroxycholecalciferol (1 alpha-OHD3) and 1,24-dihydroxycholecalciferol (1,24 (OH) 2D3). Endocrinol Jpn 1985; 32: 305-15.
72. Lindsay R, Tohme JF. Estrogen treatment of patients with established postmenopausal osteoporosis. Obstet Gynecol 1990; 76: 290-5.
73. Christiansen C, Riis BJ. 17 Beta-estradiol and continuous norethisterone: a unique treatment for established osteoporosis in elderly women. J Clin Endocrinol Metab 1990; 71/4: 836-41.
74. Mazzuoli GF, Passeri M, Gennari C et al. Effects of salmon calcitonin in postmenopausal osteoporosis: a controlled double-blind clinical study. Calcif Tissue Int 1986; 38: 3-8.
75. Overgaard K, Riis BJ, Christiansen C, Hansen MA. Effect of salcatonin given intranasally on early postmenopausal bone loss by intranasal calcitonin. Lancet 1987; ii/8574: 1481-3.
76. Reginster JY. Calcitonin for prevention and treatment of osteoporosis. Am J Med 1993; 95 (suppl 5a): 44-7.
77. Storm T, Thamsborg G, Steiniche T et al. Effect of intermittent cyclical etidronate therapy on bone mass and fracture rate in women with postmenopausal osteoporosis. N Engl J Med 1990; 322: 1265-71.
78. Watts NB, Harris ST, Genant HK et al. Intermittent cyclical etidronate treatment of postmenopausal osteoporosis. N Engl J Med 1990; 323: 73-9.
79. Reginster JY, Deroisy R, Denis D et al. Prevention of postmenopausal bone loss by tiludronate. Lancet 1989; ii: 1469-71.
80. Valkema R, Papapoulis SE, Vismans FE et al. A four year continuous gain in bone mass in APD-treated osteoporosis. In: Christiansen C, Johnsen J, Riis B, eds. Osteoporosis 1987. Glostrup, Denmark: Alborg Stiftsbogtrykkeri, 1987; 36-9.
81. Farley JR, Wergedal JE, Baylink DJ. Fluoride directly stimulates proliferation and alkaline phosphatase activity of bone forming cells. Science 1983; 22: 330-2.
82. Riggs BL, Hodgson SF, O'Fallon WM et al. Effect of fluoride treatment on the fracture rate in postmenopausal women with osteoporosis. N Engl J Med 1990; 322/12: 802-9.
83. Mamelle N, Meunier PJ, Dusan R et al. Risk-benefit ratio of sodium fluoride treatment in primary vertebral osteoporosis. Lancet 1988; ii: 361-4.
84. Baud CA, Very JM, Courvoisier B. Biophysicial studies of bone mineral in biopsies of osteoporotic patients before and after long-term treatment with fluoride. Bone 1988; 9: 361-5.
85. Gutteridge GH, Price RI, Nicholson GC et al. Fluoride in osteoporotic vertebral fracture: trabecular increase, vertebral protection, femoral fracture. In: Christiansen C, Arnaud CD, Nordin BEC et al., eds. Osteoporosis 1984. Glostrup, Denmark: Aalborg Stiftsbogtrykkeri, 1984; 705-7.
86. Hedlund EH, Gallagher JC. Increased incidence of hip fracture in osteoporotic women treated with sodium fluoride. J Bone Miner Res 1989; 4: 223-5.